Pulmonary fibrosis is a chronic, progressive, and fatal interstitial lung disease, but there is currently no effective treatment that can improve the prognosis of patients. In this blog, I would like to introduce the research results “Isolation, Characterization, and Anti-Idiopathic Pulmonary Fibrosis Activity of a Fucoidan from Costaria crostata” by Sijie Wei et al, which isolates fucoidan derived from C. costata of Costa Rica (CCP) and investigates its activity against idiopathic fibrosis both in vitro and in vivo.
First, Chemical composition analysis revealed that C. costata polysaccharide (CCP) was composed of galactose and fucose as the major monosaccharides with a sulfate content of 18.54%.
Epithelial-mesenchymal transition (EMT) is a process by which terminally polarized epithelial cells transform into mesenchymal cells. During this transformation, damaged epithelial cells change into fibroblasts and myofibroblasts, and the cells acquire migratory ability while losing the regenerative capacity of normal epithelial cells. TGF-β1 plays an important role in the EMT process. TGF-β1 is used as an inducer to transform polygonal epithelial cells into spindle fibroblasts. Therefore, A549 cells were induced with 10 ng/mL TGF-β1 and incubated with CCP (200 μg/mL) or SB431542 (4 μM) for 36 hours. After this treatment, Human non-small cell lung cancer cells (A549 cells) were subjected to a cytotoxicity assay using MTT. Compared with the blank control group, the cell viability in the TGF-β1-induced group, TGF-β1 + SB431542 group, and TGF-β1 + CCP-induced group decreased by 5.24%, 2.37%, and 3.64%, respectively.
To investigate whether CCP can inhibit EMT, cell migration and invasion abilities were evaluated by the wound-healing assay. The results showed that cell migration was dramatically increased in TGF-β1-induced cells compared with A549 cells, and the enhanced migration ability of EMT could be inhibited to various degrees by SB431542 or CCP treatment. From the perspective of cell migration, we demonstrated that CCP can inhibit TGF-induced EMT in A549 cells.
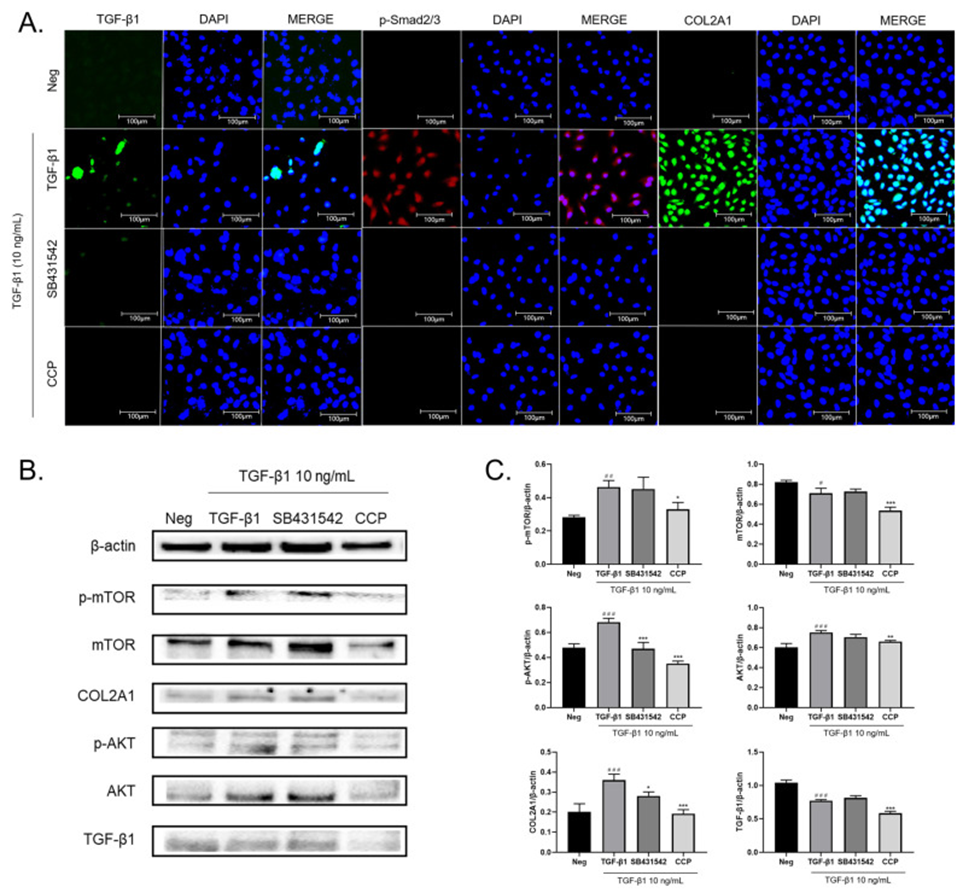
Next, using immunofluorescence, they found that TGF-β1 induction significantly increased the expression levels of TGF-β1, p-Smad 2/3, and COL2A1 in A549 cells, whereas SB431542 or CCP treatment reduced the expression of these cytokines (Figure 1A), suggesting that CCP may promote the occurrence of EMT in lung cancer via TGF-β/Smad and its downstream molecular mechanisms.
As shown in Figures 1B, and C, TGF-β1 induction significantly increased the expression of TGF-β1, COL2A1, mTOR, p-mTOR, AKT, and p-AKT. CCP treatment significantly suppressed the increase in protein expression caused by TGF-β1, while the reducing effect of SB431542 treatment was not statistically significant for p-mTOR, mTOR, and AKT.
This result is consistent with the immunofluorescence results, indicating that CCP attenuates the TGF-β1-induced EMT phenomenon in A549 cells by inhibiting the PI3K/AKT/mTOR and TGF-β1/Smad pathways.
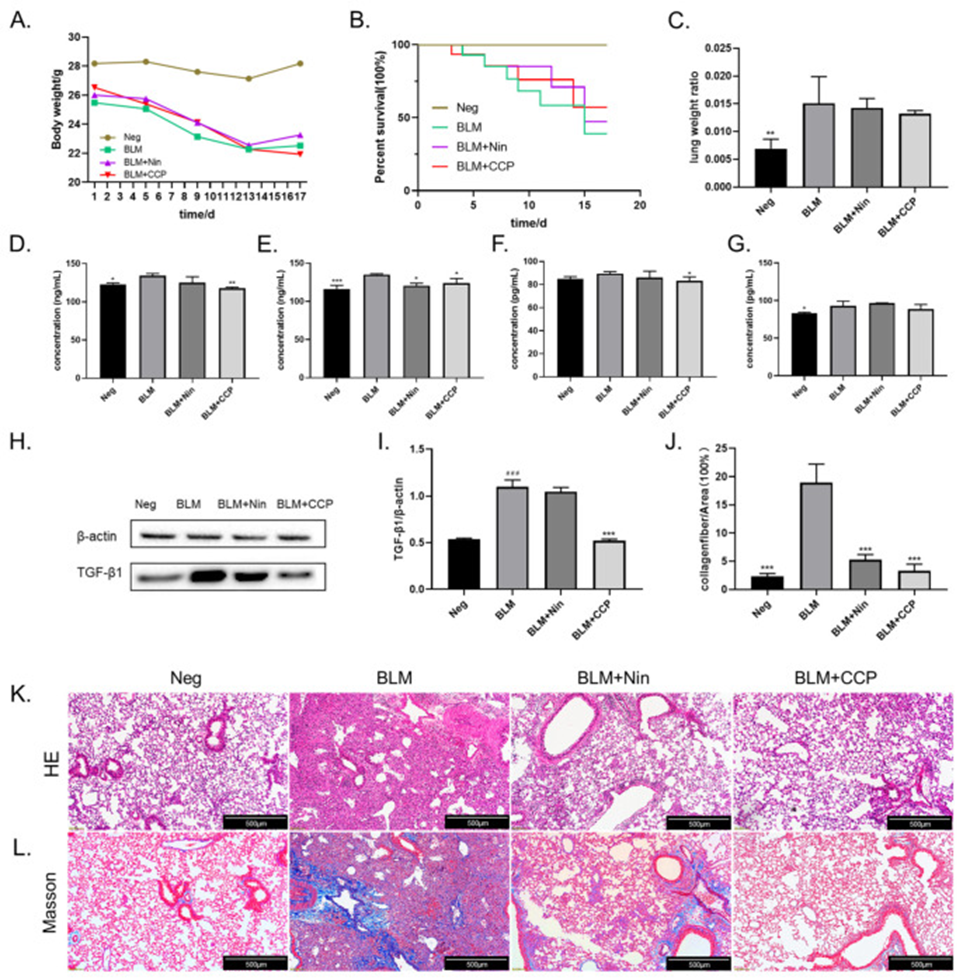
Intratracheal instillation of bleomycin (BLM) to rapidly induce pulmonary fibrosis (PF) was utilized to establish a well-defined PF mouse model, a classical method. The mice’s weight was reduced between 1 and 13 days after surgery, with the BLM-induced mice showing the greatest weight loss and the CCP-induced mice showing the smallest weight loss. The weights of all groups except the CCP group stopped decreasing after the 13th day. In the control group, the weights maintained normal levels. This suggests that the surgery caused some weight loss in the mice, which was alleviated by CCP treatment. In terms of survival rate, the survival rate of the untreated negative group (Neg) was 100%, the survival rate of the BLM-induced mice (BLM) was the lowest, the survival rate of the Nin-treated group (BLM + Nin) was the next lowest, and the survival rate of the CCP-treated mice was the highest among the different groups of surgically treated mice (Fig. 5B). In addition, the lung weight ratio of the mice after dissection was also calculated. Due to the inflammatory response and fluid infiltration in the lungs, they found that BLM induction significantly increased the lung weight ratio in mice compared with the Neg group, while the lung weight was reduced in the Nin and CCP treatment groups (Fig. 2C).
Overexpression of TGF-β1 in lung tissues of IPF patients is often a key feature. Therefore, the TGF-β1 concentration in the alveolar lavage fluid of mice was examined by enzyme-linked immunosorbent assay (ELISA) (Fig. 2D). TGF-β1 expression was increased in BLM-induced mice compared with the BLM group, and decreased in Nin- and CCP-treated mice, and TGF-β1 expression in serum showed similar results (Fig. 2E). Because the development of IPF is often accompanied by an inflammatory response and IL6-JAK2-STAT3/STAT1 is known to be an important mechanism for the effective treatment of IPF, we examined the IL-6 concentration in the alveolar perfusate and serum of mice, respectively, and showed that compared with BLM-induced mice, CCP significantly reduced IL-6 expression (Fig. 2F, G). TGF-β1 expression in mouse lung tissue was measured by Western blotting (Fig. 2H, I). The results showed that the expression of TGF-β1 was significantly increased in the BLM group.
To evaluate the histopathological changes in lung tissue, HE is staining and Masson staining was performed on mouse lung sections on the 17th day after BLM injection (Figure 2K). In the negative group, the alveolar space structure was intact, and the thickness of the alveolar compartment was normal. This revealed that BLM can cause severe alveolar and interstitial damage accompanied by inflammation and severe pulmonary fibrosis lesions. After CCP and Nin treatment, the pathological changes in the lungs were improved. There was less cell proliferation and less damage to the alveolar area and lung structure. The results of Masson staining (Figure 2L) indicate that BLM injection caused excessive deposition of mature collagen in the lungs of mice. After CCP and Nin treatment, collagen deposition was significantly reduced compared with the BLM group, but a small amount of collagen was still found in the Nin group. Quantitative analysis of Masson staining results (Figure 5J) showed that the percentage of collagen was reduced by 13.67% and 16.01%, respectively, in the Nin- and CCP-treated groups compared with the BLM group.
In conclusion, this study suggests that CCP can protect the lung from fibrosis by reducing the EMT process and inflammation in lung cells.
Source: Molecules. 2023 May 25;28(11):4343. doi: 10.3390/molecules28114343
